Does Weather Affect Pain?
By Nethra Koushik
If you ask a fibromyalgia patient whether changes in weather affect their quality of life, their answer is likely to be a resounding “Yes!” However, if you ask a doctor the same question, they would probably say something like, “That’s just a placebo.” Why is that?
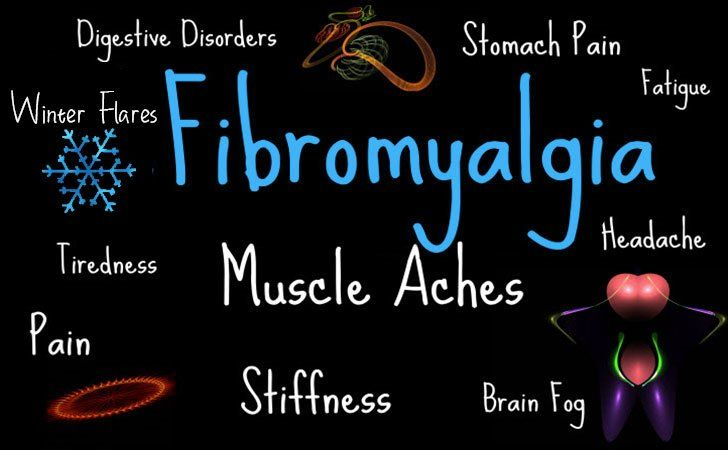
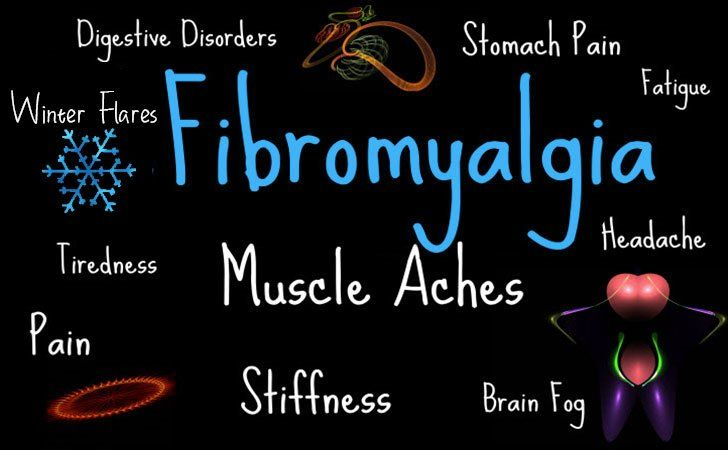
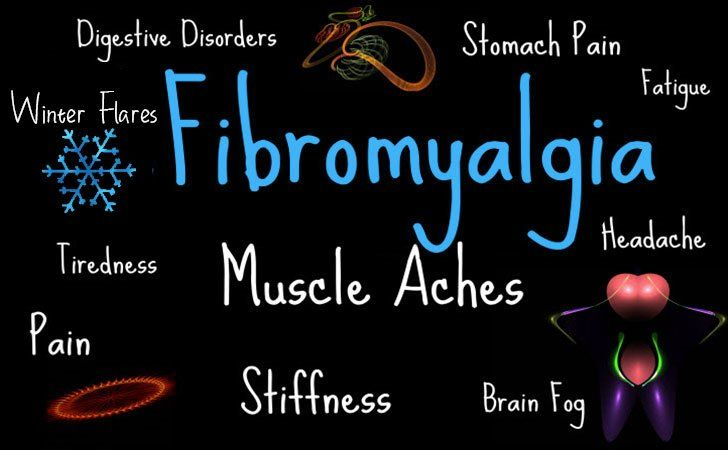
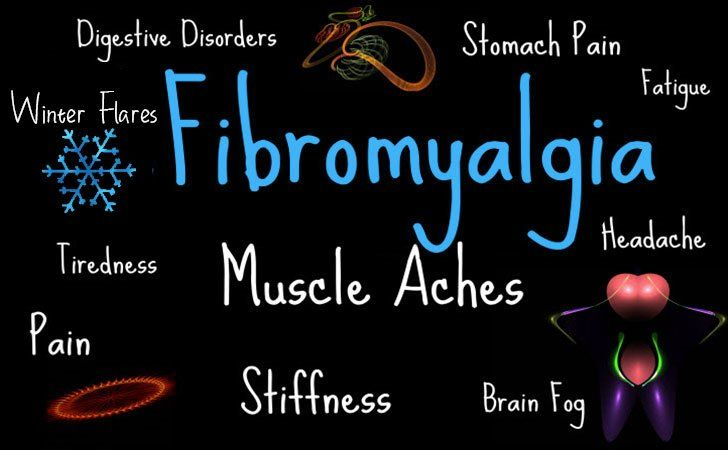
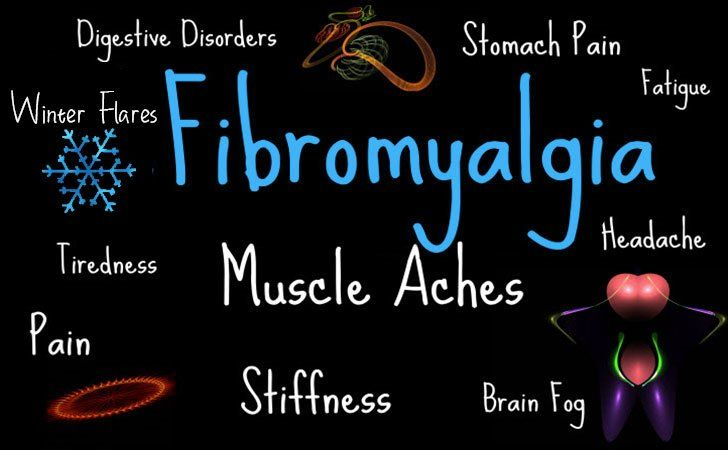
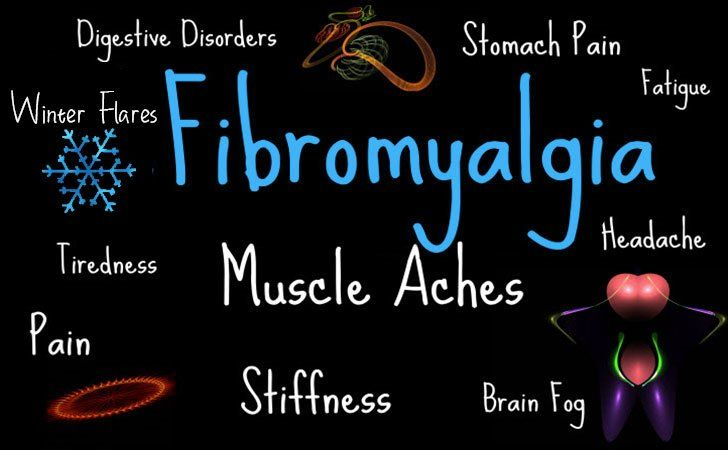
In order to answer that question, one must first explore the definition of fibromyalgia. Fibromyalgia is a chronic disorder where pain signals are amplified by the nervous system, causing muscle pain and fatigue. It is known to affect more than 600 million people around the world and is unidentifiable using objective blood or imaging tests, making it diagnosable only using subjective criteria and crossing off other possible conditions. While symptoms can be managed using medications, therapy, and lifestyle changes, there is no definitive cure. Fibromyalgia can be triggered by both genetic and environmental factors, including certain infections, stress, and weather changes.
Much research has not been conducted about the correlation between fibromyalgia and weather changes, but studies often display conflicting results.
One group of researchers set out to study the relationship between weather sensitivity and fibromyalgia symptoms (Hayashi et al., 2021). Weather sensitivity is a mood disorder characterized by physical reactions to climatic changes. These reactions can manifest as fatigue, irritability, headaches, inability to sleep, dizziness, and depression. The study asked 64 patients to provide measures of their weather sensitivity using self-perceived symptoms. They rated their average pain intensity for the day on the 0-10 Numerical Rating Scale (NRS), with 0 being “no pain” and 10 being “worst possible pain.” They also rated their quality of life on the Euro-Quality of Life-5 Dimensions-3 Level (EQ-5D-3L) scale, which has a range of -0.111 to 1.000. Here, negative ratings signify conditions worse than being dead, 0 signifies death, and 1.000 signifies being healthy. Whether the patients were weather-sensitive or not was determined using a simple “yes” or “no” question: “Do changes in weather affect your pain?” The results were then compared and analyzed to determine whether a patient’s quality of life is affected by weather sensitivity.
Put simply: it is. Or at least that is what the results of this particular study showed. The NRS and EQ-5D-3L scale values of those with weather sensitivity were significantly worse than for the people without. The difference in NRS and EQ-5D-3L values showed that the difference in pain intensity between groups was 1.5 points, while their quality of life varied by 0.16 points.
So if there is a strong correlation between the two, why do so many professionals dismiss it?
Despite the strong correlation between weather sensitivity and increased pain in patients, some major issues in the study could not be overlooked. For instance, the minimum clinically important difference for NRS values is 2 points. However, the present study exhibited a difference of fewer than 1.5 points, rendering the association too minimal to be considered clinically significant. While weather changes affected patients on an individual level, the correlation was simply not strong enough to deem this a conclusive study. Second of all, the sample size – only 64 patients – was too small to make an accurate conclusion. Furthermore, the researchers measured weather sensitivity solely using reports based on self-perceived symptoms by the patient, which is largely prone to subjectivity and errors.
On the other hand, some studies directly opposed the results of the one at hand. For example, a Norwegian study performed by E.A. Fors and H. Sexton examined the correlation between the pain symptoms of 55 females and weather over the course of 28 days (Fors, 2002). The results were inconclusive, showing that changes in weather do not predict the severity of pain. Researchers were also unable to pinpoint exactly what type of weather worsens symptoms. The study addressed its discrepancies; one being how it might have been better to measure pain in the morning or evening instead of 2:00 p.m – which is the time period where patients reported the least symptoms. Patients with pre-existing mental health conditions, like depression or anxiety, are also more likely to report higher pain intensity, making the study liable to subjective error. Interestingly, further analysis of the results showed that newly diagnosed patients often complained of their pain worsening with weather changes, while the symptoms of older patients showed no correlation. Researchers were unable to discover scientific reasons for this and began to examine the possibility that the pre-conceived notion of weather worsening pain affects patients more than the weather itself.
However, there is no denying that the pain these patients feel is very real — and for a disease with no cure, healthcare providers must be equipped to treat the symptoms to the best of their abilities. Conducting more extensive studies with a greater number of subjects and more objective testing could help put an end to this debate so that patients can get the treatment they deserve.
References
Hayashi, K., Miki, K., Hayashi, N., Hashimoto, R., & Yukioka, M. (2021). Weather sensitivity associated with quality of life in patients with fibromyalgia.
BMC Rheumatology, 5(1).
https://doi.org/10.1186/s41927-021-00185-4
Fors, E. A. (2002). Weather and the pain in fibromyalgia: are they related?
Annals of the Rheumatic Diseases, 61(3), 247–250.
https://doi.org/10.1136/ard.61.3.247