Pain is an alarm system. This alarm rings at any indication of damaged tissue, flushing electrophysiological signals towards our brain like fire through weeds. Humans learn to respond to pain by avoiding any future actions that could stimulate the same reaction or cause the same wounds. Sometimes, however, there is no wound, and yet the alarm system still rings.
When pain seems to persist past normal healing time and acts continuously, it is categorized as chronic. Up to 20% of people in developed countries suffer from chronic pain. As opposed to acute pain, where the cause of the sensation is localized, chronic pain is often persistent and does not stem from one treatable source.1 The onset of chronic pain often begins with specific conditions such as back and neck injuries, osteoarthritis, fibromyalgia, post-surgical pain, and more.2 However, instead of a natural recovery, chronic pain typically lingers and can often be a life sentence.
Chronic pain can often fall into two categories. One of these forms of pain is induced by nerve damage, called neuropathic pain. Sometimes, neuropathic pain is traced to an issue with pain receptors, which are parts of cells that exist solely to transmit the feeling of pain; these specific cases are called nociceptive pain.3 Ultimately, chronic pain has historically been an ambiguous medical categorization for a dysfunction not fully understood.
How We Understand Chronic Pain
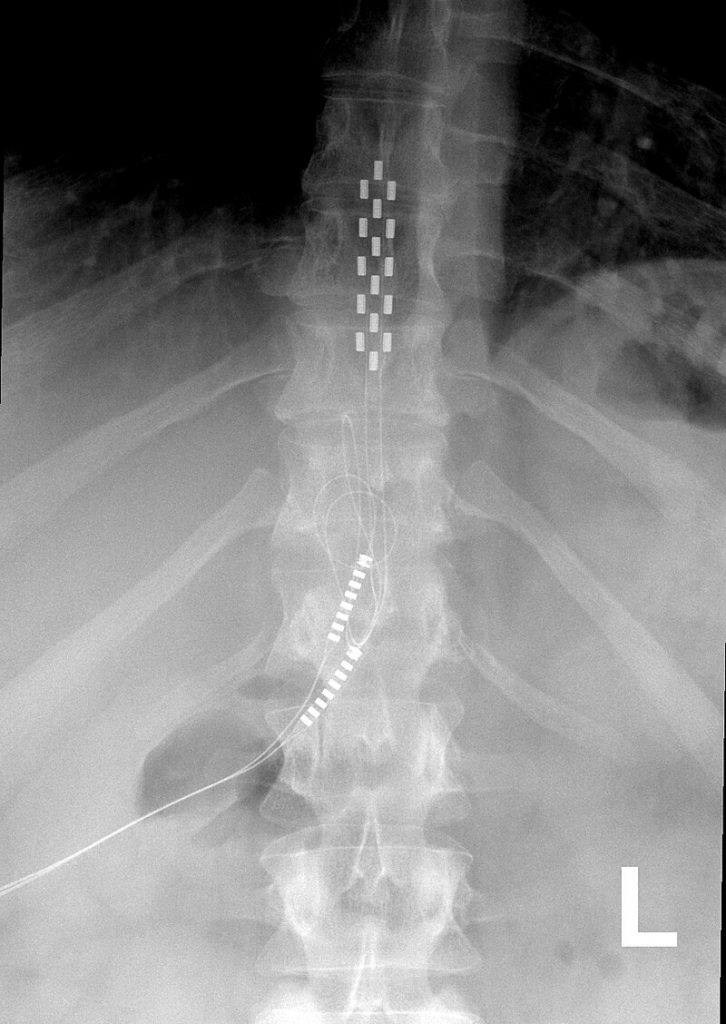
To say chronic pain elicits frustration is an understatement. For both patients and doctors, there is an expectation to cure that which generally cannot be localized and physically treated. The treatments for chronic pain that do exist are typically not long-lasting or may lead to addiction and distress. Chronic pain is deeply intertwined with issues such as the opioid epidemic, in which patients have developed addictions to pain-relieving drugs.4 Furthermore, recent technologies such as spinal cord stimulation (see Figure 1) continuously dishearten patients when they do not permanently cure their pain.1
Chronic pain, as such, is latent with stories of dependence and disappointment. This is especially seen in high impact patients, for whom the pain affects daily activity. In many cases, to be a victim of chronic pain is to be subject to seemingly endless physical and emotional tribulations. Researchers have begun to recognize this binary—the physiological side and the psychological side. The recognition of the latter dimension has rapidly opened doors in pursuit of methods to treat chronic pain. The field has taken a sharp redirection towards interdisciplinary cognitive studies, modeling chronic pain in both neurological and psychological conditions.
The Neurological
One of the largest frustrations in chronic pain patients stems from an inability to communicate symptoms to professionals, or a fear of not being believed by statutory agencies.2 Because there is no external lesion or injury to point to, the internal experience is robbed of its validity when unknowing individuals doubt its existence. However, recent studies highlight the very real neurological dimension of chronic pain.5
In a paper by Farmer et al. in 2012, researchers centered their study around the basis of behaviorism: a psychological theory that orients human behavior as being learned through positive and negative reinforcement, like the classic study of Pavlov’s dog trained to know it was time to eat when it heard a bell ring. Built upon this premise, the study used a brain scanning technology called functional magnetic resonance imaging (fMRI) to observe a predictable pattern in a part of the brain associated with experienced pain, dubbed the “Pain Neuromatrix.”5
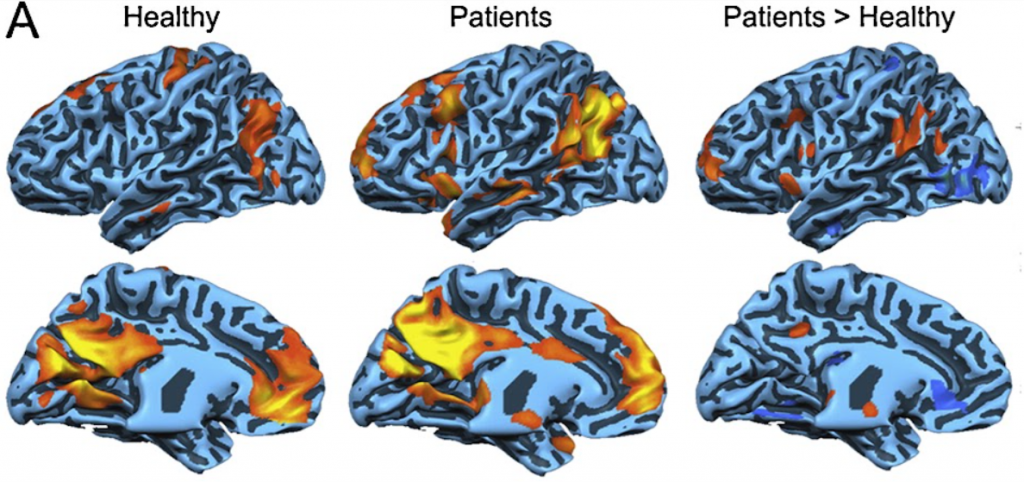
They found that in chronic pain patients, this Pain Neuromatrix is continuously stimulated. The stimulations regularly follow a certain path that becomes normalized and essentially carved out for easy access to future stimulations. With time, the neural networks shift from sensory to hedonic brain circuitry, meaning the brain has reworked its sense of aversion and rewards. It will prioritize the neural network that it is most familiar with: the pain pathway. Functional changes occur in the underlying structure of the brain, so that even when at rest, there is increased activity in pain-related regions (see Figure 2). Through this conditioning process, chronic pain is physically inscribed into the brain so that the networks triggered by acute pain are more prone to being stimulated—even when there is no external reason for acute pain to be registered.5
The Psychological
The behaviorist modeling of chronic pain extends past the brain’s physical conditioning. With the field’s cognitive approach, psychological and sociological frameworks are integral to understanding the onset, proliferation, and treatment of chronic pain. Not only does the context of an individual’s life influence the role chronic pain plays, but certain rationalizations and behaviors can also reinforce and develop the physical feeling of the pain itself.6
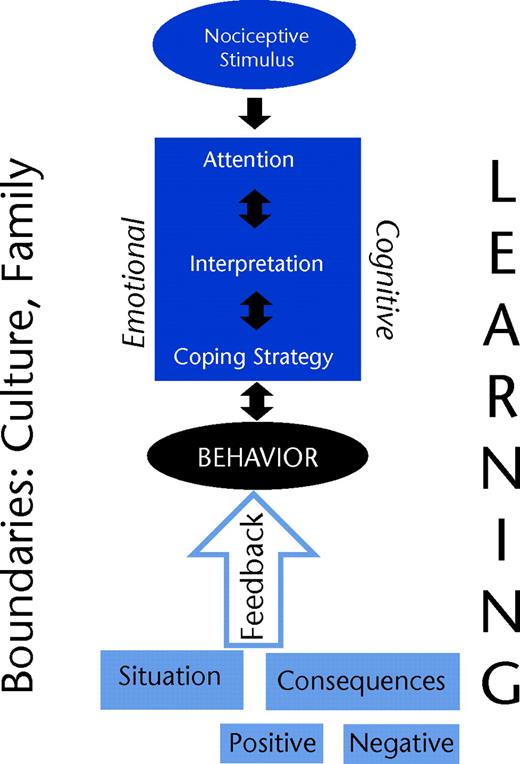
There are a plethora of models that frame the potential actions and behaviors that can influence chronic pain. One such model suggests that attention forces us to focus on the pain, our cognitions will shape our interpretations of that pain, our emotions and emotional regulation will prompt how we react, and our overt behavior reinforces our perception of the pain. A visual representation of this model is seen in Figure 3.6
One example of these factors at play is the fear-avoidance model. In such a model, patients understand that pain usually indicates something is wrong with their health. Therefore, they are afraid to worsen the issue and opt to remain immobile. Because most doctors encourage patients to remain active and learn to adapt to the pain, this decision may worsen the feeling of pain and the patient’s quality of life. Their tendency to catastrophize and worry about the worst possible outcome in turn enacts a self-fulfilling prophecy. Believing some prediction to be true, they inadvertently make the prophecy come true.6
The psychological dimension of pain reveals just how subjective the experience may be, as not everyone will rationalize and respond to pain in the same way, affecting the perception of the pain itself.
Cognitive Treatments
There is not an explicit cure to chronic pain, but in centralizing its psychological dimension, potential cognitive behavioral therapies become apparent. This has been a recent approach in the realm of pain clinics, which are multidisciplinary treatment centers for those experiencing chronic pain. In the United States alone, there are said to be around 2000 clinics, most of which employ a broad range of both psychological and physical treatments.7
Pain clinic physicians do not aim to eliminate the pain of their patients, but rather to help redefine the role of pain in their lives by promoting physical activity and reconditioning, as well as learning behavioral coping skills. They often introduce patients to their mode of treatment by telling them they are not helpless in dealing with the pain nor do they need pain to define their lives and futures.7
Each patient’s treatment plan looks different because every patient’s pain looks different—even if it stems from the same condition and there is no externally visible issue to point to. It is with this redirection of chronic pain modeling that patients can potentially change their interpretations, emotions, and behavior responding to pain, and in turn, alter the perception and intensity of their pain as a whole.
While a long-lasting cure to chronic pain remains unknown, medical professionals have continuously offered new ways of approaching various conditions by shifting their paradigms in interpretations and treatments. The proliferation of biopsychological frameworks offers mitigation of chronic pain’s overwhelming nature—an interim while specific treatments more in line with spinal cord stimulation develop to offer more tangible solutions. In the meantime, chronic pain patients have the opportunity for a downstream solution: one which does not stop the condition at its source, but ultimately still makes life with chronic pain more manageable.
Acknowledgements
I would like to thank Professor Catherine Cahill of the UCLA Psychiatry and Biobehavioral Sciences department for reviewing this article and ensuring its clarity and scientific accuracy. I would also like to thank Aashi Parikh and Luyang Zhang, the Berkeley Scientific Journal Features editors, for their guidance and support.
References
- Sinclair, C., Verrills, P., & Barnard, A. (2016). A review of spinal cord stimulation systems for chronic pain. Journal of Pain Research, Volume 9, 481–492. https://doi.org/10.2147/jpr.s108884
- Dow, C. M., Roche, P. A., & Ziebland, S. (2012). Talk of frustration in the narratives of people with chronic pain. Chronic Illness, 8(3), 176–191. https://doi.org/10.1177/1742395312443692
- Bridgestock, C., & Rae, C. P. (2013). Anatomy, physiology and pharmacology of pain. Anaesthesia & Intensive Care Medicine, 14(11), 480-483.
- Højsted, J., & Sjøgren, P. (2007). Addiction to opioids in chronic pain patients: A literature review. European Journal of Pain, 11(5), 490–518. https://doi.org/10.1016/j.ejpain.2006.08.004
- Farmer, M. A., Baliki, M. N., & Apkarian, A. V. (2012). A dynamic network perspective of chronic pain. Neuroscience letters, 520(2), 197-203.
- Linton, S. J., & Shaw, W. S. (2011). Impact of psychological factors in the experience of pain. Physical therapy, 91(5), 700-711.
- Turk, D. C., & Meichenbaum, D. (2017). A cognitive-behavioral approach to pain management. In The evolution of cognitive behavior therapy (pp. 132-154). Routledge.
Image References
Banner Image: Picryl. (n.d.). Ladislav Mednyanszky – Old Man’s Death. Death of the Painter’s Father. https://picryl.com/media/ladislav-mednyanszky-old-mans-death-death-of-the-painters-father-o-3135-slovak-1a4340
Figure 1: Spinal cord stimulator. (2022, October 9). Wikipedia. https://en.wikipedia.org/wiki/Spinal_cord_stimulator
Figure 2: Farmer, M. A., Baliki, M. N., & Apkarian, A. V. (2012). A dynamic network perspective of chronic pain. Neuroscience letters, 520(2), 197-203.
Figure 3: Linton, S. J., & Shaw, W. S. (2011). Impact of psychological factors in the experience of pain. Physical therapy, 91(5), 700-711.
